It has taken NIH eight full years to complete their intramural study on Myalgic Encephalomyelitis (or what NIH calls “ME/CFS”) and publish their paper “Deep phenotypic of post-infectious myalgic encephalomyelitis/chronic fatigue syndrome.” I take no pleasure in the fact that some of us accurately predicted the outcome of this study to be a delivery vehicle for the introduction of a new psych label for ME—which turned out to be the concept of effort preference—re-branding post-exertional malaise (PEM) and pacing as psychological.
The burying of ME has been going on for a long time at both NIH and CDC. Patients need to learn from this instead of giving NIH the benefit of the doubt because the agency has proven, over decades, that it would be foolish and dangerous to do that. However, even without awareness of that history, it would be difficult not to see the serious flaws in this paper. What follows is a truncated analysis of some of the issues.
Concerns Materialized
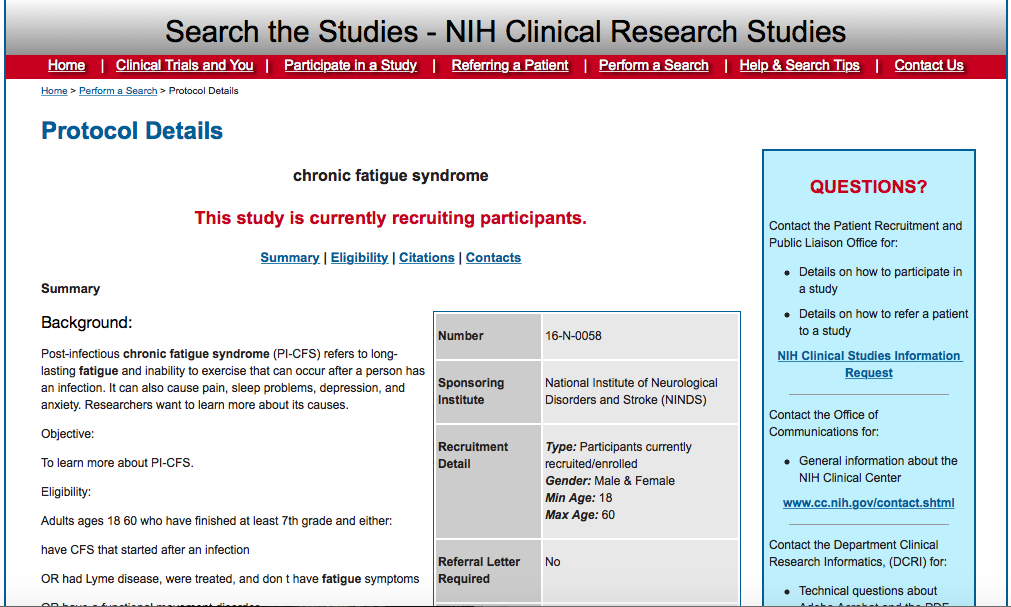
Advocates’ and patients’ main concern from the outset was the historic bias on the part of NIH against acceptance that ME is an organic disease process rather than a vague syndrome of fatigue and malaise. ME patients experience a dramatic loss of health and function that is both severe and persistent. NIH has never taken ME seriously by investing in research that would look in earnest for the cause of this loss. In the case of this study, the key concerns were that NIH would 1) use overly inclusive criteria to select a heterogenous patient group resulting in meaningless data, 2) use a small patient cohort that would produce statistically irrelevant results, 3) put researchers with an agenda in charge of the study, who would disregard or disrespect the scientific method, the large number of abnormal biological findings by renowned researchers in the field, and the experience and knowledge of patients, and 4) perpetuate or even expand the institutional bias against ME as an organic disease in favor of a psychological disorder. The latter two threats loomed particularly large in light of NIH’s involving of Dr. Brian Walitt, an extremist ME denier, who has been vocal for many years with his unsupported view that ME is somatoform. The actual outcome is an exponential step in the wrong direction due to the NIH’s confirming and even exceeding all of our concerns.
The ME community extensively protested numerous aspects of the NIH intramural study in 2016 with some limited success. For example, the community’s protest prevented NIH’s inclusion of a control group of patients with Functional Movement Disorder, a form of Functional Neurological Disorder. That initial plan immediately tipped the community off as to NIH’s agenda of classifying ME as functional or otherwise psychological. Another win was the removal from the study of Dr. Fred Gill, a proponent of Graded Exercise Therapy and Cognitive Behavioral Therapy for ME patients
Unspecific Criteria, Mixing and Matching of Criteria
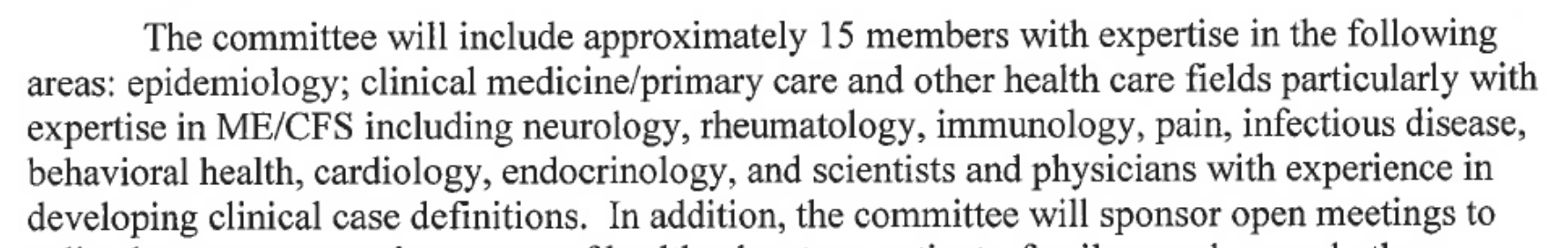
We were also able to head off the use for patient selection of the 2005 Reeves Criteria, a preposterously over-inclusive definition of ME that would have guaranteed the participation of patients who do not actually have ME, e.g., patients with idiopathic fatigue, primary depression, etc. However, NIH used two other overly broad and unspecific definitions, one being the 2015 criteria of the former Institute of Medicine (IOM). The IOM redefinition of ME—a government-sponsored project, which many patients with untreated sleep disorder would satisfy due to the definition’s reliance on self-reporting and its lack of exclusions—was the subject of one of the largest ME-community protests, which included an open letter to the Secretary of HHS signed by more than fifty experts in the field and objecting to the redefinition of ME by non-experts, such as the IOM panel stacked with a considerable number, about half, of non-experts. Moreover, the IOM committee members were emphatic in their instructions that the IOM riteria were not to be used in research precisely because they do not guard against selecting the wrong cohort, a fatal blow to any research.
NIH’s use of the IOM definition in their intramural study constituted exactly the kind of bait and switch that independent advocates had been warning about with respect to the IOM definition. NIH, as the world’s premier medical research institution, which had bankrolled the new IOM definition, was, of course, acutely aware of the impropriety of using the IOM criteria. Similarly, the Fukuda Criteria, also used for patient selection in this study, tend to capture a large number of patients who do not have ME, not unlike the Reeves Criteria.
Why would NIH attempt to use the most unspecific U.S. criteria, Reeves, for patient selection and not even consider—despite changing study criteria at least five times in the process of designing this study—the strictest criteria available, the 2011 International Consensus Criteria written by ME experts, which would seem to be desirable in any ME research but especially at an institution of NIH’s reputation in research of a disease that the agency had abandoned for decades? Why was the agency afraid to study the most robust cohort?
And why did NIH use three different definitions in this study, the third one being the experts’ Canadian Consensus Criteria of 2003 (CCC)? I have seen ME studies that require that each participating patient meet each of several different criteria, although I have often wondered why those researchers would not just use the strictest of those criteria. If I had to take a guess, the inclusion of the IOM Criteria in particular but also the use of Fukuda is probably a nod to the CDC and NIH in hopes of securing future NIH funding by including government-sponsored definitions. However, the situation here is different: patients had to meet just one of the three definitions, not all of them. So, basically, NIH was studying three different, not comparable cohorts without differentiating them, potentially leading to studying unlike patient groups as if they were the same and, therefore, making the entire study suspect.
It is true that ME experts acted as adjudicators in the patient-selection process, but as far as I know, all those adjudicators were involved in ME research at the time and were likely vying for NIH grants and, therefore, not likely to risk antagonizing NIH. More importantly, Walitt was the one pre-screening patients, providing an opportunity to skew patient selection in a way that favors the inclusion of patients with a less classic ME profile or worse, which apparently is exactly what happened. The study authors’ self-serving claim that they “used rigorous criteria to recruit” ME patients, clearly untrue, casts doubts on their other claims.
When NIH felt the heat from independent advocates and patients in 2016, they promised that all participating patients would have to meet the CCC and be objectively tested for PEM in an effort to quash the criticism.
This was once again a bait and switch because NIH kept neither of these commitments. For example, only nine patients met the CCC, the strictest criteria used. In case there was any doubt as to the broad nature of the IOM Criteria, all seventeen ME patients met that definition. Fukuda was not far behind with fourteen patients.
Moreover, patients were not objectively tested for PEM before enrollment to rule out misdiagnoses. Self-reports of PEM are often undependable; therefore, relying on them is an unscientific approach when an objective test is available. Two-day CPETs are the gold standard for identifying such exacerbation, and NIH’s refusal to require them as part of the cohort-selection process is illuminating. Research by questionnaires will not result in science deserving of the label.
Statistically Irrelevant Cohort Size
The extremely small cohort size was another concern for many independent advocates. The study was originally designed for forty ME patients, a disproportionately small number for a disease that the CDC has been claiming for nearly two decades afflicts millions in this country. Because this study was on the NIH’s back-burner, it was completed years after the original projected completion date of 2018 and ultimately included only seventeen ME patients, a farcical cohort size that basically constitutes statistical gaslighting. The agency claims that this delay and downsizing were due to the COVID pandemic, a claim that does not hold up on further examination as the study was supposed to be completed well before the beginning of the pandemic. In any event, it would be naive to underestimate the impact of an NIH paper no matter how underpowered it is.
Importantly, the paper claims that four of the seventeen selected patients, or about twenty-five percent, spontaneously recovered. Because the usual recovery rate in ME (if there are any true recoveries as opposed to misdiagnoses or patients adjusting their expectations as to what healthy is) is much smaller at around five percent, some or all of those four patients might have been improperly selected. Frankly, such a high number of purported recoveries raises questions about the ME diagnosis of the other participants. Moreover, the paper’s inclusion of the four allegedly recovered subjects’ data is dubious and calls into question the validity of the entire paper.
Ridiculing of Patients
There were a number of other indicators of NIH’s antagonistic attitude toward ME, including the fact that the researchers involved, other than Walitt, obviously wanted nothing to do with ME and apparently viewed their involvement as a hardship assignment. The research team expressed their resentment by dubbing themselves “Team Tired,” a deeply ableist and demeaning name that foreshadowed the effort-preference outcome and confirmed that the institutional bias vis-a-vis ME that has been entrenched at NIH for decades is alive and well.
Dr. Brian Walitt
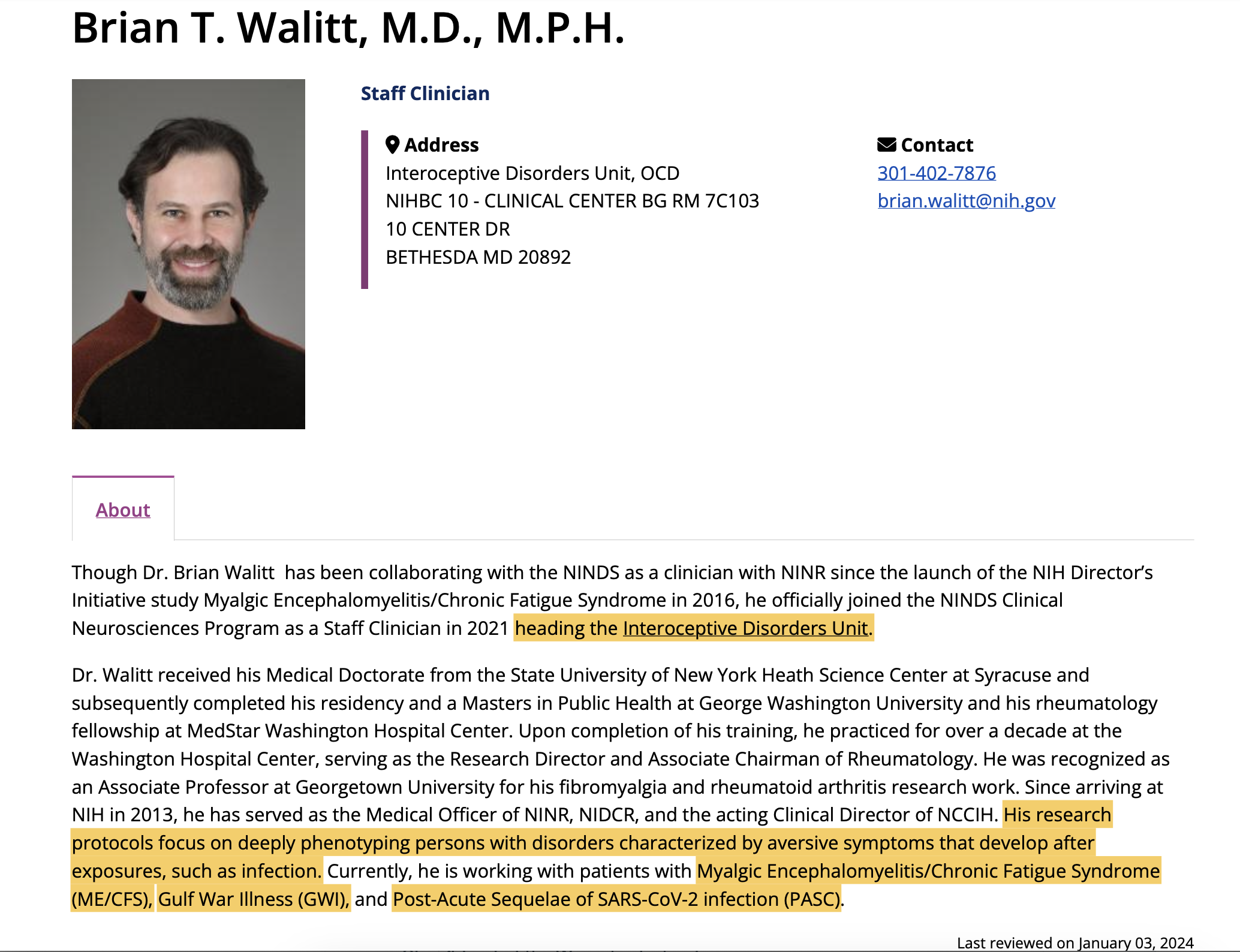
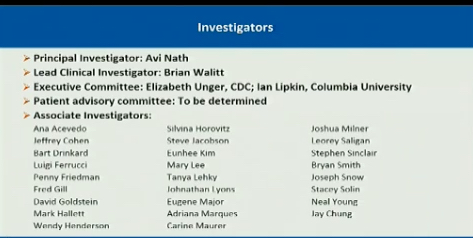
NIH’s Dr. Brian Walitt was the Lead Associate Investigator and Lead Author of the paper who designed the study protocol, pre-screened patients for participation, and made the day-to-day decisions in this study.
In a 2016 NIH ME advocacy call, Walitt famously claimed that he has no bias—not just no bias vis-a-vis ME, but no bias at all—which is rich given that Walitt is an acolyte of British psychiatrist Dr. Simon Wessely and medical historian and professor of psychiatry Edward Shorter, leading, obstinate, and prolific proponents of the disgraced and discarded theory of a biopsyschosocial origin of ME, and others in the biopsyschosocial school.
The similarities between Wessely and Walitt are striking and plentiful, for example:
Wessely in 1994:
“I will argue that M.E. is simply a belief, the belief that one has an illness called M.E.”
“The experience of fibromyalgia is very much real to the people who have it.”
There is a similar resemblance between the views of Walitt and Shorter, who devoted an entire book, From Paralysis to Fatigue, to the history of psychosomatic illness, which in his view includes ME. Naturally, it was Walitt who invited Shorter for a talk at NIH in 2016. This heavily criticized event was staunchly defended by Dr. Walter Koroshetz, Director of the National Institute of Neurological Disorders and Stroke (NINDS). Koroshetz argued that the invitation did not constitute an endorsement as though providing Shorter with an NIH pulpit is harmless. Would NIH have invited Andrew Wakefield? Koroshetz’s feigned obtuseness fooled nobody given the not subtle similitude of Shorter’s and Walitt’s views.
As is the case with Wessely, there is an endless supply of execrable Shorter quotes regarding ME. Here is just one:
Patients’ groups and physician-enthusiasts of CFS have seized with glee a trickle of inchoate immunological findings.… Quite naturally, psychosomatic patients who want their symptoms to keep abreast of scientific progress wish to see the underlying source of their problems as immunological in nature.
Long-time independent advocate Liz Willow aptly characterized Walitt in a recent tweet:
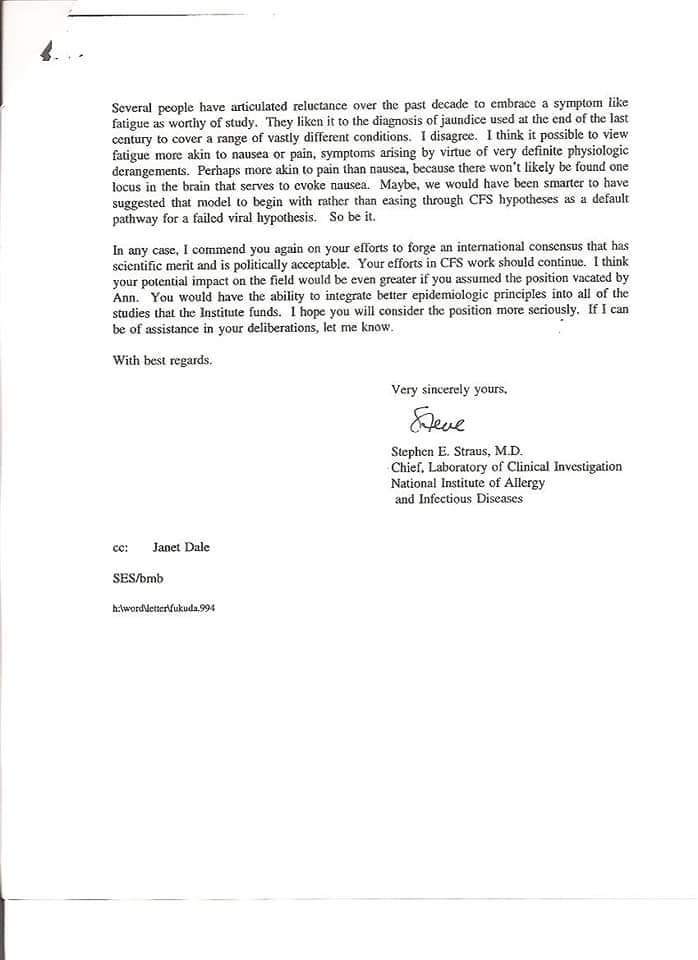
Dr. Stephen Straus was the architect of the concept of ME as mere “Chronic Fatigue,” which concept has since permeated all federal health agencies, most notably the CDC and NIH. As reported by the late ME advocate Craig Maupin as a result of a Freedom of Information Act request, author of the blog The CFS Report, Straus is on record in a memo to the CDC’s Dr. Fukuda (of the 1994 Fukuda Criteria) as to his hope and plan of reducing ME—a complex multi-system disease with many severe symptoms, fatigue not being the defining one—to mere fatigue as the result of the then-new Fukuda Criteria. Straus predicted that “the notion of a discrete form of fatiguing illnesses will evaporate. We would then be left with Chronic Fatigue that can be distinguished as Idiopathic or Secondary to an identifiable medical or psychiatric disorder.” Straus sounded elated when he concluded this fantasy with, “I consider this a desirable outcome.” In other words, the goal of the most prominent ME researcher at NIH in the 1980s and 1990s was the abandonment of ME, and nothing seems to have changed at NIH more than three decades later as Walitt carefully traces Straus’s footsteps.
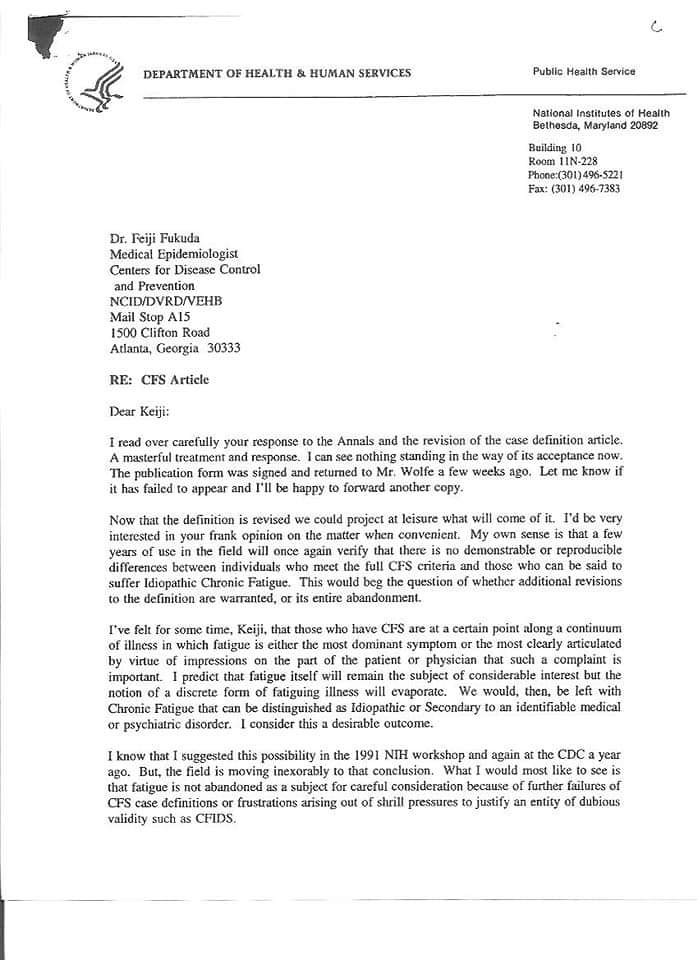
 Moreover, Straus was dismissive of findings of immunological abnormalities in ME. He also considered ME to be on a “continuum of illnesses in which fatigue is either the most dominant symptom or the most clearly articulated.” That is exactly Walitt’s position when he considers ME and Fibromyalgia to be all but identical, their diagnosis merely hingeing on “what [patients] complain about”:
Moreover, Straus was dismissive of findings of immunological abnormalities in ME. He also considered ME to be on a “continuum of illnesses in which fatigue is either the most dominant symptom or the most clearly articulated.” That is exactly Walitt’s position when he considers ME and Fibromyalgia to be all but identical, their diagnosis merely hingeing on “what [patients] complain about”:
The complaint that predominates your existence is how you end up being named, which has nothing to do with your physiology.
That is who pre-screened ME patients for intramural NIH study, somebody who might as well have thrown darts for patients selection. And once again, Walitt finds himself supported by Wessely:
The distinction between fibromyalgia and CFS is largely arbitrary and both overlap with affective disorder.
According to ME expert Dr. Byron Hyde, Straus was even verbally violent and threatening toward ME patients in person at a CDC meeting in Atlanta (start listening at 4:20). This was still not enough for NIH to remove him from ME research.
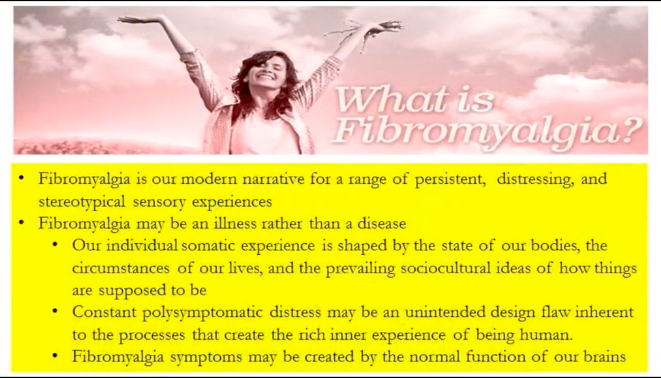
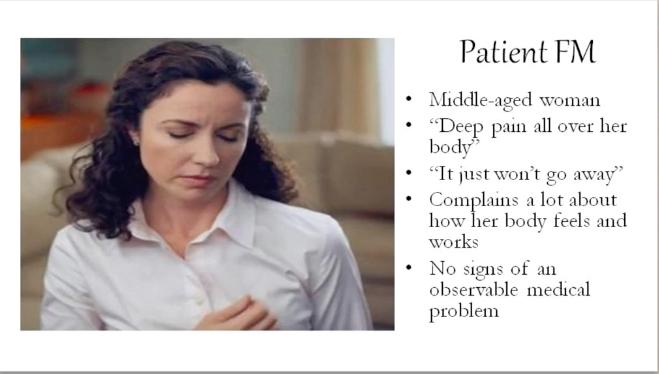
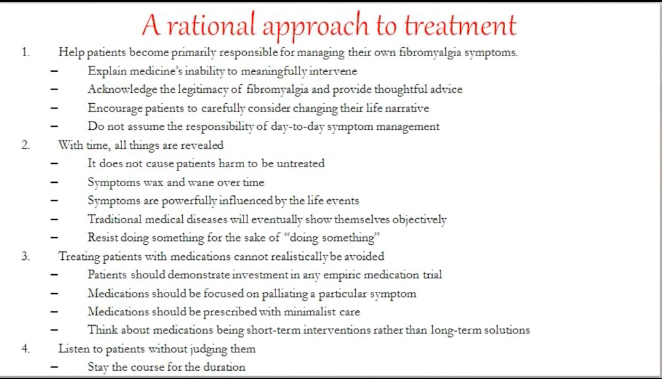
As a rheumatologist, Walitt infiltrated and embedded himself into the world of ME (and now also Long COVID and Gulf War Illness) via Fibromyalgia. Although Walitt seemed to be doing a reasonable, though ultimately unconvincing, job feigning compassion toward his Fibromyalcgia patients, whom he paraded around in his presentations like circus attractions, his unhinged views are aggressively hostile toward ME and Fibromyaliga patients; he has been vocal with his conclusory view that both ME and Fibromyalgia are somatoform.
The discordance between the severity of subjective experience and that of objective impairment is the hallmark of somatoform illnesses, such as fibromyalgia and chronic fatigue syndrome.
For well over a decade now, Walitt has been establishing himself as an ME and Fibromyalgia enemy who considers the symptoms of ME and Fibromyalgia as within the “range of normal” and not worthy of validation or treatment because, in his opinion, they do not constitute medical entities. What is abnormal, in his view, is the patients’ beliefs that they are suffering from a disease. As if it is not bad enough that an NIH researcher has been allowed to build a career on such propaganda, Walitt works hard to convert his colleagues whom he claims are relieved that they no longer have to pretend that Fibromyalgia is pathological after he “say[s] [his] message.” This disturbing ten-minute Walitt interview about Fibromyalgia will leave little to the imagination in terms of Walitt’s predisposition. I analyzed the ghastly views he expressed in this interview when independent advocates protested his involvement with the study.
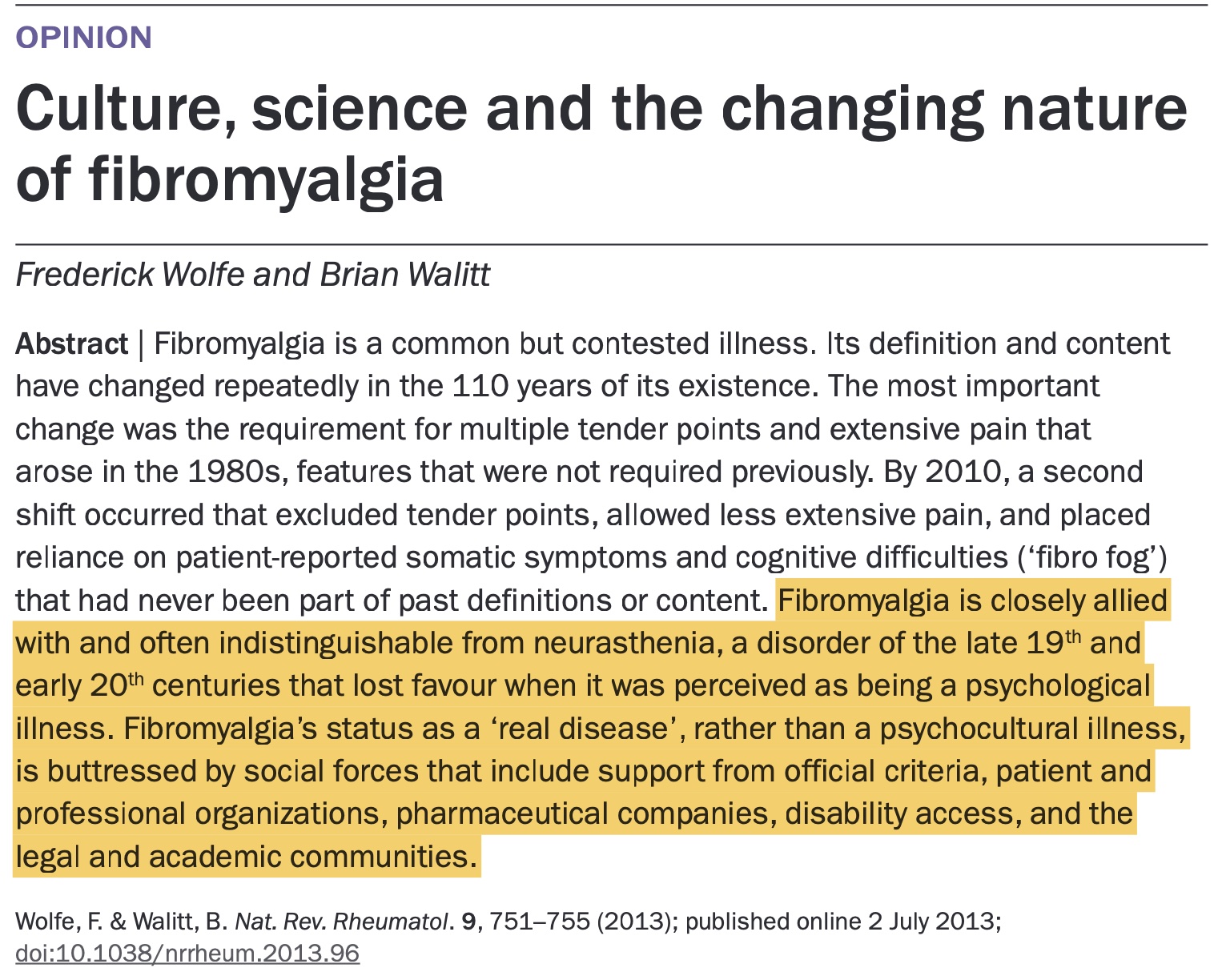
Another good example of Walitt’s disturbed views on Fibromyalgia and ME is an opinion paper that he co-authored with his biopsychosocial soulmate, the late Dr. Frederick Wolfe: “Culture, science and the changing nature of fibromyalgia.” Somebody saved a copy of this paper on the Wayback Machine.
In this paper, in which he quotes Wessely and Shorter, Walitt equates Fibromyalgia with Neurasthenia—i.e., “the vapors,” “depression of spirit,” “hypochondriac affections,” “effort syndrome,” etc. Neurasthenia is a psychologized fatigue concept that had started out as a central-nervous-system disorder and was the predecessor of Holmes’s and Fukuda’s “CFS.” Walitt referred to Wessely’s framing of ME as Neurasthenia in the slick and insidious “Old wine in new bottles: neurasthenia and M.E.” In his paper, Walitt expresses his belief (no science required) that Fibromyalgia is psychocultural, i.e., “shaped primarily by psychological factors and societal influences” and is associated/comorbid with psychological illness. Throughout the paper, Walitt labels Fibromyalgia—in addition to psychocultural—psychological, psychogenic, psychosomatic, a Somatic Symptom Disorder (i.e., somatoform), a social construct, etc. He further claims that Fibromyalgia is related to psychological disorders (including major psychopathologies), psychosomatic symptoms, and personality disorders and that it is a convenient, because socially acceptable, diagnosis for mentally ill patients to hide behind. According to Walitt, Fibromyalgia patients are not to be trusted because they have too many symptoms that are too severe and too unusual while appearing too healthy resulting in physicians’ shunning of them. Walitt laments the failure of Fibromyalgia as a psychological concept and strongly disapproves of what he calls the “success” of Fibromyalgia. He sounds practically paranoid when he blames “powerful societal forces,” which he claims have been “marshalled,” for propping up the “‘real disease’ message.” Walitt frames Fibromyalgia as a con job by patients and patient organizations whom he claims were enabled by other malevolent actors and forces, such the American College of Rheumatology (guilty for naming and defining it), governments, disability and pension systems, physicians, the legal and academic communities, scientific organizations, pharmaceutical companies, the Internet, and ICD codes. That’s an impressive list. Imagine if patients indeed had the allyship of those stakeholders and systems! There is no other characterization of Walitt’s Fibromyalgia views than deranged. And, of course, because ME and Fibromyalgia are basically the same to him, all of this applies to ME according to Walitt’s twisted views.
As sordid as the government’s record regarding ME has been, the intramural NIH study has opened a new, even darker chapter for patients. Putting Walitt in charge of this study despite his unmistakable bias against ME patients is just one item on a long list evidencing an atrocious track record on the part of the federal health agencies, including NIH, when it comes to ME. It warrants a reminder that there have been calls by federal health officials to silence critical patient voices as well as actual threats against members of CFSAC—the since dissolved federal Chronic Fatigue Syndrome Advisory Committee—who refused to toe the party line in addition to many actions by federal officials designed to thwart patient advocacy.
Walitt’s unyielding belief that ME, Fibromyalgia, and other diseases are reflections of an incorrect inner understanding of patient body’s capabilities seems to have grown only stronger over the years. His extremism will likely be weaponized against patients for decades to come unless NIH stops involving him in these studies. So far, NIH has circled the wagons to defend him and even promoted him by moving him from the National Institute of Nursing Research (NINR) to the more prestigious NINDS and making him head of the Interoceptive Disorders Unit.
NIH’s unconscionable insistence on putting a researcher in charge who propagates at NIH and elsewhere that ME does not even exist sends a chilling and unambiguous signal that the agency is committed to going down the biopsychosocial rabbit hole with the unmistakable goal of discrediting ME and ultimately discarding it as a medical entity altogether, which is just what Walitt has been lobbying for inspired by his role model Straus.
Effort Preference
Functional and Somatoform
The community’s worst concern materialized. All protestations of Nath and NIH surrogates in the media to the contrary, this study marks a renewed effort meant to lay the groundwork for NIH’s and CDC’s official categorizing of ME as psychological after decades of working toward that goal.
Just as the advoctes predicted, NIH attached a new psychological label to ME: effort preference. According to NIH, “[T]hese findings suggest that effort preference, not fatigue, is the defining motor behavior of this illness.” (Advocates, of course, agree that fatigue is not the defining symptom of ME, but what NIH was really getting at is that there is no muscle fatigue in ME.) The paper also asserts, somewhat inconsistently, “Fatigue is defined by effort preferences and central autonomic dysfunction.” NIH defined effort preference as “the decision to avoid the harder task” or “how much effort a person subjectively wants to exert.” The term effort preference—featured prominently in the Abstract and used twenty-six times throughout the paper, i.e., a major aspect of the study’s outcome—indicates a choice on the part of patients in how active they are. That part of the paper is an abomination and has already caused and will continue to cause great harm to patients who face prejudice, neglect, ridicule, and abuse on a regular basis.
From the start, NIH was committed to finding a functional angle in ME as evidenced by their attempt to include patients with Functional Movement Disorder, a common sub-type of Functional Neurological Disorder, as a control group, seemingly an effort at reverse-engineering their desired outcome. This quote from the paper seems to be saying functional as well: “Considering all the data together, PI-ME/CFS appears to be a centrally mediated disorder.” This is a conclusion at which NIH arrived after allegedly finding reduced brain activity in the right temporal-parietal area (TPJ). The paper claims:
This decreased brain activity is experienced as physical and psychological symptoms and impacts effort preferences.
And then there was the NIH media blitz following the publication of the paper with the agency hammering home the functional-disorder message. Dr. Nath said:
We did not find any structural abnormalities but multiple functional abnormalities.
and
It’s a functional suppression; it’s not a structural damage.
So, the brain of ME patients is not working properly, but NIH found no reason for that malfunction. Ergo, the functional classification, which in light of NIH’s limited, flawed, and biased inquiry is entirely unsupported. How can the study simultaneously find that patients prefer to exert themselves less than they safely can but also that their brain is limiting their ability to exert themselves? After all, effort preference and effort intolerance are mutually exclusive. Is it a choice or not? Were they lying then, or are they lying now?
If you are thinking “no structural damage” cannot be a good thing for ME patients, you would be correct and not just from a scientific-progress perspective. Classifying ME as functional is psychologizing it. Just think of how patients are faring who have a Functional Neurological Disorder (formerly Conversion Disorder) diagnosis, which is listed as a mental illness in the DSM-5. To assess ME patients’ effort-based decision-making, NIH used the Effort-Expenditure for Rewards Task (EEfRT), an alleged measurement of motivation and anhedonia, which is the core symptom of Major Depressive Disorder. Why would NIH even investigate a psychological model of ME while refusing to perform a second-day CPET if it were indeed committed to science?
In the context of NIH’s claim of having found only functional abnormalities and no structural abnormalities, consider Walitt’s historical emphasis on the dual function of the brain: biological and psychological. According to him, the symptoms of patients with fibromyalgia and ME are the result of normal brain function, i.e., not of structural abnormalities. Although Walitt acknowledges that patients believe that their symptoms indicate that they are sick, he claims that those symptoms are not a sign of abnormal biology indicative of disease.
But what NIH has done with the effort-preference model of ME goes further than stigmatizing patients with a functional label. NIH claims that they did not find any muscle fatigue as the underlying cause for the decline in performance of ME patients. In other words, according to NIH, ME patients limit their effort due to unwarranted concerns about PEM despite their bodies, in fact, not being prevented by an organic cause from performing harder tasks. That is a textbook case of a somatoform disorder (technically now captured as Somatic Symptom Disorder in the DSM-5), a disorder characterized by physical symptoms accompanied by an excessive amount of time, energy, emotion, and/or behavior related to the symptom that results in significant distress and/or dysfunction. If patients’ bodies are not actually dictating that they stay within strict limits, then their pacing by staying within safer limits and thereby severely curtailing their lives surely would constitute an excessive and dysfunctional focus on their symptoms. Of course, Functional Neurological Disorder has historically also been considered a sub-category of somatoform disorders. NIH’s fancy footwork in the paper itself and particularly in the media cannot cover up the new psych label that they pinned on ME.
Crucially, the presence of many biological abnormalities in ME patients does not rule out a somatoform disorder because symptoms do not have to be medically unexplained to fit the DSM-5 diagnosis of Somatic Symptom Disorder. Once caught in the somatoform searchlights, patients cannot escape them no matter how well adjusted they are. The more that patients point to their numerous abnormal test results, the more they are faulted for their alleged obsession with their symptoms as if they are pulled down by quicksand. What a carefully constructed, treacherous catch-22!
It is self-evident that Walitt is responsible for the effort-preference hit job. When you compare the psych language historically used by him—“discordance between the severity of subjective experience and that of objective impairment is the hallmark of somatoform illnesses, such as … chronic fatigue syndrome”—with the soundbite he gave to the NIH press office regarding the NIH paper, it tracks one hundred percent:
In other words, the psych part of the study was pre-determined by NIH’s putting Walitt in charge.
It would be interesting to hear NIH explain how an effort preference leads to enlarged lymph nodes, elevated viral titers, abnormal two-day CPETs, abnormal SPECT scans, etc. Moreover, given their effort-preference rubbish, should patients not be getting better instead of crashing when they push themselves past their safer limits as they often have to because life demands it?
NIH’s solidifying of its stance that ME is a psychological disorder will send an unambiguous signal to researchers who seek funding for biomedical studies not to submit grant proposals to NIH that are inconsistent with a functional or somatoform or another psychological angle of ME. It is already nearly impossible for independent researchers to obtain NIH funding for ME studies focused on physiological causes and mitigations. This study might well slam the door on experts in the field, who have advanced the science of ME dramatically, unlike NIH, because extramural researchers may now be prevented from continuing to do so and from replicating ME research.
No Muscle Fatigue
Participating in this study was obviously grueling for patients and likely involved travel for many of them and more than one trip to the NIH facility for some. In other words, patients who were properly diagnosed with ME were probably experiencing PEM by the time they arrived at NIH and certainly once testing began. Nevertheless, the paper rules out the possibility that the subjects’ decline in performance was caused by muscle fatigue, even though the data does not validly support that claim. Several tests were performed that relate to the effort-preference claim. None of them involved the entire minute ME-patient cohort, and the only test that even attempted, through the use of electromyography, to determine whether the declining performance of ME patients was due to muscle fatigue as opposed to avoidance behavior involved only eight ME patients. Add to that the issues with patient selection (What are the odds that those electromyography patients met CCC?), and the effort-preference claim is not only unrelated to science; it is hostile to science.
This raises the question, why would NIH even consider publishing this paper, which brands ME patients with a sweeping and obviously manufactured psych label based on a perversion of science? I understand the motive of Walitt: unfounded psych claims are the fuel on which his career advancement feeds. Unfortunately, there is no other way to interpret NIH’s decision to publish this train-wreck than that NIH shares Walitt’s agenda.
The effort-preference concept revived the pernicious notions of “fear of exercise” and “avoidance behavior” and pathologized pacing, without which patients continue to deteriorate. The resemblance of those discredited concepts and effort preference tracks with Walitt’s favored research area: aversive symptoms that develop after certain triggers, such as infections.
For years, patients were urging the government to study PEM. The federal health agencies refused to even acknowledge PEM until that became untenable in light of the strong science around two-day CPETs. They then pivoted to blaming patients for not pacing properly when they crashed. Now, they found a way to weaponize PEM by claiming that patients just think that they are crashed, but their brain is mistaken. NIH has taken one of the major ME symptoms—the exacerbation of symptoms after exertion or what NIH calls effort sensitivity—and redefined and psychologized it by bastardizing science.
Of note, even the one-day CPET was performed on only eight ME patients. NIH’s decision not to adopt the gold-standard two-day CPET allowed them to claim that patients are deconditioned. They knew that a second CPET would clearly show a significant drop-off and, thus, refute the implication that deconditioning is involved in patients’ disability. A second-day test would also have dropped a grenade into their effort-preference game plan, and that is likely why NIH shied away from it, not financial constraints at half a million dollars per patient and not feigned concern for patients’ wellbeing as they claimed.
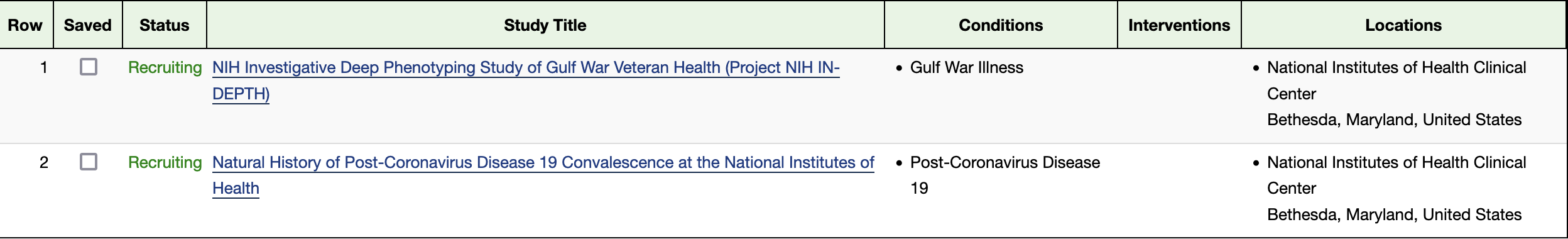
Implications for Long COVID
There is an obvious effort at NIH to increasingly platform Walitt prominently with respect to ME, Long COVID, and Gulf War Illness despite deafening advocate protests. Although the science is not there yet to show that PEM-like Long COVID is identical to ME—and many in the ME community, including eminent researchers in the field, certainly have their doubts about that—NIH seems to consider them basically the same. So, with that backdrop, it is important to note that Walitt is the principal investigator for ongoing intramural Long COVID and Gulf War Illness studies at NIH, and I believe that those communities should brace themselves for an outcome of their NIH studies that will be similar to the ME paper in terms of a new psychological label.
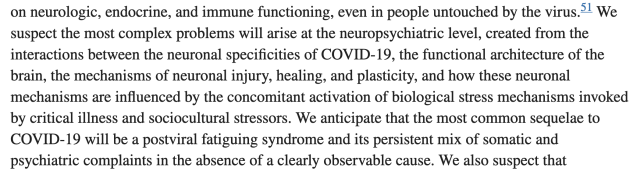
Walitt has a habit of giving previews of his future studies, which apparently is how NIH does science these days. In his paper “A clinical primer for the expected and potential post-COVID-19 syndromes,” he is predicting that he will find sociocultrual stressors (I sense an effort to be more refined with his euphemisms since the days when he called Fibromyalgia pyschocultural) as well as neuropsychiatric and psychiatric issues. In addition, he is prophesying issues with the functional architecture of the brain, just like NIH claims to have uncovered with respect to ME. Whatever Walitt’s Long COVID studies will cost the taxpayer will be merely to buy the appearance of science and validity, not to actually to do legitimate science. Here is a screenshot of part of the paper’s conclusions:
It is untenable for NIH to continue involving Walitt in any ME, Fibromyalgia, Long COVID, and Gulf War Illness studies. If the agency nevertheless does so, they are sending a clear signal. Empowering obviously extremist researchers is not an accident.
I realize that this requires a difficult adjustment reaction, but I would strongly caution Long COVID patients against believing that what happened to ME patients over many decades could or would not happen to Long COVID patients. That would be a dangerously rose-colored view of the state of affairs that underestimates both the agenda and the power of the biopsychosocial school. Wessely disciples, such as Walitt, have mercilessly built successful careers on the backs of ME and other patients, and they will not hesitate to bring Long COVID under their psych umbrella. The only chance Long COVID patients have is getting out in front of this and starting to protest Walitt’s involvement now. Once the Walitt Long COVID paper is published, it will be too late, and his appointment as principal investigator of an ongoing NIH Long COVID study, for which he is currently recruiting patients, means that Long COVID advocates will come from behind on this.
I, therefore, urge Long COVID patients to coalesce as many patients as possible (using appropriate caution to protect their health) as well as healthy allies to prevent NIH’s leveraging of the intramural ME study in their intramural Long COVID study. This will be an existential fight for the Long COVID community, and all stops have to be pulled out to prevent Long COVID from being buried. Long COVID has strength in numbers, and the sooner patients realize the enormity of the fight they are in for, the higher the chances that Long COVID will fare better than ME has so far. Patients and advocates have a voice and the power to affect this situation if they take it seriously and act vigorously. Their future medical care and, for some, even their lives hang in the balance.
I also encourage Long COVID patients to study the sordid ME history, no small feat. A good start would be reading Osler’s Web, the acclaimed book about the history and politics of ME written by award-winning investigative journalist and brilliant writer Hillary Johnson.
Existential Risk to ME Patients’ Income
In 2016, I warned about the potential fall-out of Walitt’s involvement in this study with respect to patients’ benefits. Psychologizing ME as the NIH intramural study has done poses dangers on many fronts (medical treatment, support from family and friends, presentation of ME in the media, contamination of research, etc.), but I cannot overemphasize the danger to patients’ long-term disability benefits, which generally are limited to twenty-four months for disabilities caused or contributed to by mental/nervous disorders, including psychological disorders; this includes any health issues allegedly presenting with the psychological concept of effort preference. Contrast that with disability benefits not involving mental-health aspects, which extend until retirement age or recovery. Already approved patients who are past the twenty-four-months mark are no less at risk. Due to the frequent abuse by insurers of the standard mental-health limitation in long-term disability policies, it has always been exceedingly difficult for ME patients to get approved for long-term disability benefits beyond twenty four months, but the intramural NIH study is all but guaranteed to make that now exponentially harder if not impossible, having provided ammunition to insurers against patients of which insurers will undoubtedly make good use.
Conclusion
This NIH study is a damning case study on flawed methodology. Worse than the methodological flaws of the study is NIH’s obvious biopsychosocial ME agenda confirming its decades-old institutional bias of ME as a psychological disorder. Letting Walitt run the study made this outcome a foregone conclusion. Had this been private-sector research in any field, the research team would have known better than to publish this paper or else have reason for serious concern about reputational damage for being affiliated with a study that manifestly worked hard to deliver a biased and predetermined outcome. NIH lifers, obviously, do not have such concerns because of the lack of repercussions for scientific misconduct at NIH, but if any of the 75 researchers involved with this study have private-sector aspirations, having their name on this paper might turn out to be a career-limiting move unless they distance themselves from it.
In 2013, NIH bought a new ME definition from the IOM while remaining steadfast in their decades-long refusal to conduct ME research. NIH has now taken that new definition and slapped a psych label on ME patients through its intramural study—a manufactured outcome at which NIH arrived by letting somebody whose life’s mission has been to psychologize diseases such as ME look at only eight questionably selected patients. This study cost eight million dollars of taxpayer money and delivered exactly the outcome Walitt—and by association the NIH—desired: a reinvigorated campaign to dismiss ME as an organic disease. Independent advocates predicted this.
The effort-preference part of the study does not merely constitute scientific malpractice; given its implications, it amounts to scientific battery. It has the potential of becoming the PACE trial* on steroids and should be retracted immediately, but until it is, it presents a clear and present danger to ME patients, and chances are that NIH will build on their false effort-preference claim for ME and other diseases it considers related.
We must continue to protest the effort-preference outcome of this study; it cannot stand. Moreover, NIH has left no doubt that intramural ME research is harmful to patients. We need NIH to commit to substantial funding of extramural research of the numerous areas of biological abnormalities in ME by experts in the field who are committed to science. Other than funding, however, NIH needs to stay away from ME as long as it is enabling researchers who harbor Walitt-type biases. We also must call for an immediate investigation of NIH’s institutional bias against diseases such as ME, Long COVID, Gulf War Illness, and Fibromyalgia.
___________________________________________________________
*PACE is the debunked (but not yet retracted) U.K. study recommending Graded Exercise Therapy and Cognitive Behavioral Therapy for ME, which has caused immeasurable harm to patients worldwide but especially in the U.K.